HLH. 아주 흔하지 않은데 그래도 발병하기에 DDx에는 끼어넣어야하는 질환.
Introduction and epidemiology
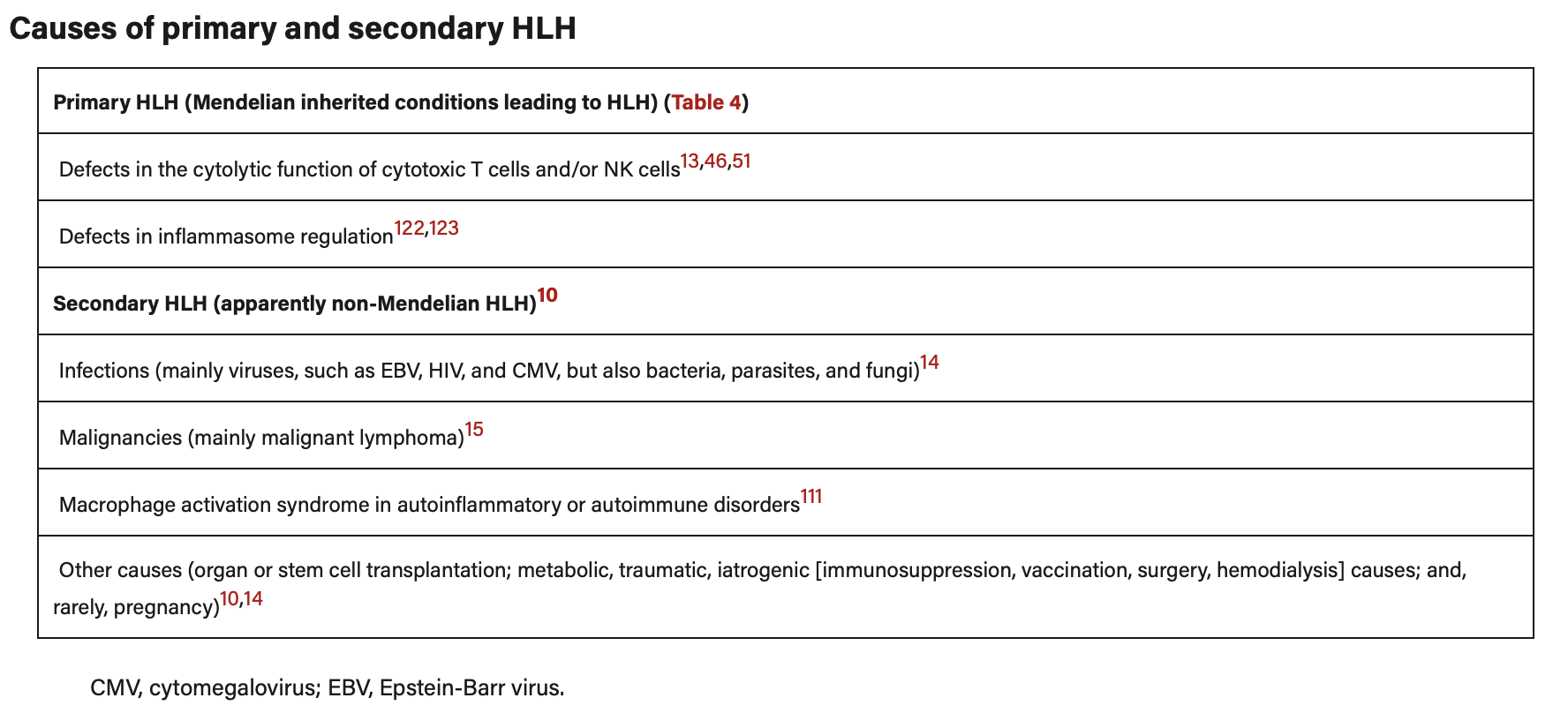
Hemophagocytic lymphohistiocytosis (HLH) is a disease with major diagnostic and therapeutic difficulties. HLH comprises two different conditions that may be difficult to distinguish from one another: a primary and a secondary form
1)Primary HLH
-The primary autosomal recessive form, familial hemophagocytic lymphohistiocytosis (FHL), has an estimated incidence of around 1:50,000 live-born children
-FHL is a fatal disease with a median survival of less than 2 months after diagnosis if untreated, and that typically has its onset during infancy or early childhood
-Despite its name, family history is often negative since the disease is recessive. Importantly, the onset of FHL and bouts of the disease may be triggered by infections
2)Secondary HLH
Secondary HLH (sHLH) may develop as a result due to strong immunological activation of the immune system, which may, for example, be caused by a severe infection. sHLH has been described in immunocompromised hosts in association with viral infections, virus-(infection) associated hemophagocytic syndrome (VAHS, or IAHS)
-However, most patients with sHLH are not obviously immunosuppressed. sHLH may also develop during malignancies (malignancy-associated hemophagocytic syndrome, MAHS); it may either be the presenting clinical picture and initially mask an underlying malignancy, or it may develop during the treatment for a known malignancy
The epidemiology of HLH varies substantially as a result of population heterogeneity and variable underlying triggers. A large literature review on adult HLH reported a mean age at HLH onset of 49 years (63% males).
The reported incidence of malignancy-associated HLH varies from 1% in patients with hematological malignancies (0.36/100 000 individuals per year) to a cumulative incidence rate of 2.8% in patients with malignant lymphoma and 9% of patients with acute myeloid leukemia (AML) after intensive induction therapy.
Pathogenesis
HLH is an aberrant hyperinflammatory hyperferritinemic immune response syndrome that is driven by T cells and associated with a potentially fatal cytokine storm.
The term “macrophage activation syndrome” (MAS; or MAS-HLH) refers to a subset of patients with HLH arising on a background of systemic autoinflammation/autoimmunity and should be restricted to patients with Still’s disease, lupus, vasculitis, and other related autoimmune systemic diseases, because its treatment may differ from that recommended for other forms of sHLH
-an inability of the immune system to adequately restrict stimulatory effects of various triggers. Inherited variations in HLH-associated genes, which are well characterized in pediatric HLH, may play a role in adult-onset HLH, but acquired immune dysfunction in response to infections, malignancies, and autoinflammatory/autoimmune disorders seems to be the leading cause in adults
HLH triggers, including occult malignancies, require a meticulous search for the underlying disease that should be continued, despite ongoing HLH treatment
Infections are the most prevalent triggers of HLH. In adults, particularly with increasing age, malignancies, primarily lymphomas, are another major cause
A variety of malignancies are associated with HLH in adults, including T-cell or natural killer (NK) cell lymphomas (35%), B-cell lymphomas (32%), leukemias (6%), Hodgkin lymphoma (6%), other hematologic neoplasms (14%), solid tumors (3%), and other nonspecified neoplasms (3%).
Diagnosis
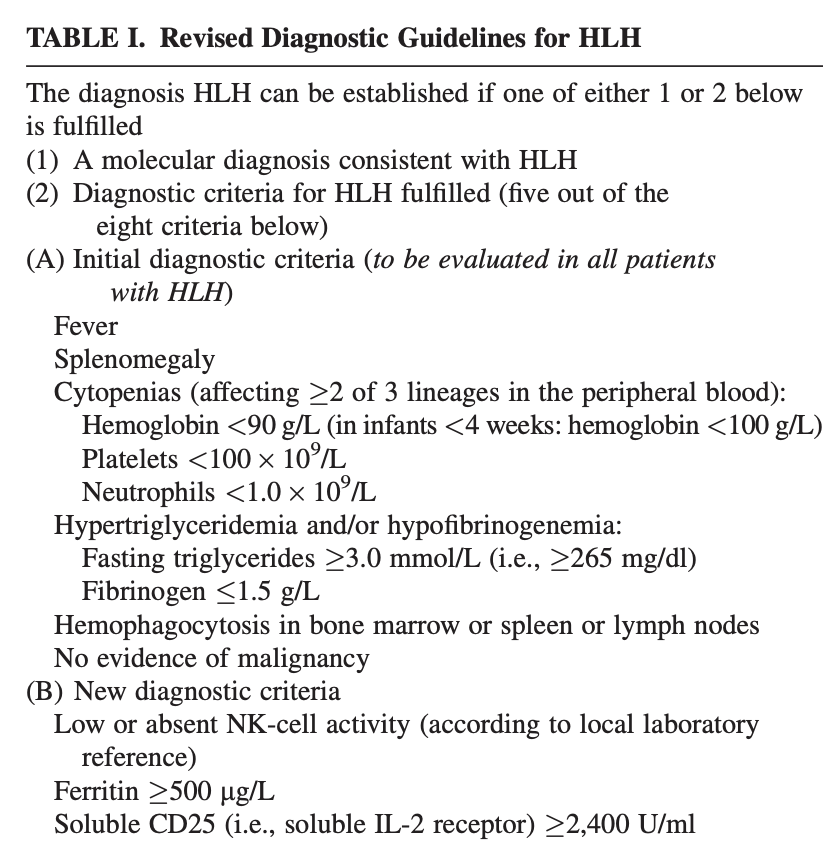
In HLH-94, the first prospective international treatment study for hemophagocytic lymphohistiocytosis (HLH), diagnosis was based on five criteria (fever, splenomegaly, bicytopenia, hypertriglyceridemia and/or hypofibrinogenemia, and hemophagocytosis).
In HLH-2004 three additional criteria are introduced; low/absent NK-cell-activity, hyperferritinemia, and high-soluble interleukin-2-receptor levels. Altogether five of these eight criteria must be fulfilled, unless family history or molecular diagnosis is consistent with HLH.
H score
Treatment
- Under Haematology care
- HLH 2004 protocol (HLH-2004 chemo-immunotherapy )
- Dexamethazome 10mg/m2 BD : control the hyperinflammatory state
- Etoposide - chemotherapeutic agent : control the hyperinflammatory state
- Cyclosporine A
- in selected patients, intrathecal therapy with methotrexate and corticosteroids.
- Subsequent hematopoietic stem cell transplantation (HSCT) is recommended for patients with familial disease or molecular diagnosis, and patients with severe and persistent, or reactivated, disease.
- IVIG 2mg/kg 24hrly - over 2 -5days (4days this time) depending on the patient's condition and tolerance
- additional courses may be required based on the patient's clinical status and response to treatment can exten over several weeks
- role in modulating the immune response and providing immunosuppression -provide passive immunity, and reduce the activity of autoreactive T-cells and macrophages.
- Daily weighs
- Bone marrow biopsy
- Daily fibrinogen, triglyceride, ferritin in addition to usual bloods
- APLS screen
- CMV and EBV NAT
- Soluble CD25
- HSV &HHV8 NAT
- UBA1
Reference
1. HLH2004: Diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis
'호주 의사 라이프:)' 카테고리의 다른 글
| Multiple myeloma 다발성 골수종 (0) | 2024.06.18 |
|---|---|
| 다계통 위축증 Multiple system atrophy (MSA) (0) | 2024.06.17 |
| Alport syndrome 알포트 증후군 (0) | 2024.06.14 |
| 항인지질증후군/항인지질항체증후군 Antiphospholipid syndrome (APLS, APS) (0) | 2024.06.13 |
| 폐색전증 Pulmonary embolism (1) | 2024.06.13 |